It’s safe to say the past few months have been incredibly busy. The last time I sat down to write an article, I had only just switched on to the second block of my rotating internship, and now I’m into my fourth. I can’t believe how quickly time is passing – it really does fly when you’re having fun.
As I sit nursing a fairly solid hangover from a lovely wedding (congratulations Jeremy and Ness), I thought it would be good to reflect on the busiest shift of my internship so far – the August bank holiday Monday.
Setting the scene
As I’ve eluded to previously, as an RVC intern I have various roles. One main job is manning the first opinion emergency service, covering the out-of-hours for around 50 practices. As you can imagine, things can get quite hectic quite quickly – especially when you consider the emergency and critical care (ECC) referrals coming through the same doors.
I have to admit, weekends at the Queen Mother Hospital for Animals (QMHA) are a tad busier than I’m used to. A culmination of high caseload, paperwork and various other intern duties meant that in my previous block, where I was working the weekend, I would routinely put in 30-plus hours over the Saturday and Sunday. Now, this isn’t in any way meant to come across like I’m complaining – after all, I chose to do this and have absolutely no regrets; I’m loving it – but I would be lying if I said those shifts weren’t tiring.
The August bank holiday is classically one of the busiest weekends of the year for the QMHA, so our rota was altered slightly to increase staffing in preparation for the Monday. We had everything planned out. Three of us would start at 8am – one would start with emergencies and the other two would get to work on the inpatients, and get their hospital sheets and plans sorted for the day. Then, another colleague would come in at noon, and a further at 2pm. Plenty. Ah, the best laid plans of mice and men.
As I turned up to morning rounds at 8am, the emergency room (ER) telephone rang to let us know an animal had just arrived and needed triaging. This patient was reported to have seizured earlier in the morning, so my triage was relatively quick and the patient was taken into our ER for observation. A few minutes later, the telephone rang again to let us know another patient, which I’ll refer to as Bubble, had arrived and was collapsed. Rounds would have to be postponed.
Prioritisation and point of care
I have previously written about the importance of rounds – they allow a proper handover of patients and help provide continuity of care at high standards. Unfortunately, in a busy ER it can be difficult to protect this time. We try our best, but new critical patients often end up being prioritised. As I got to work on trying to figure out what was wrong with my collapsed patient, I let the other two interns continue with rounds and come up with plans for the day.
No one right way to approaching a collapsed patient exists – we all have our different tips, tricks and strategies for trying to assess the major body systems. For me, after an initial major body system assessment, I often turn to ultrasound to guide my next steps.
Point-of-care ultrasound (POCUS), focused assessment with sonography for trauma (FAST)… various names exist for use of ultrasound in the ER, but all essentially document the same thing. Looking for fluid – whether pulmonary, pleural, pericardial or peritoneal – can be a rapid way of ruling in or out a lot of disease processes in our collapsed patients. I am by no means an expert, and would encourage those who are interested to consult the relevant literature, but I do really enjoy POCUS. Various protocols are discussed, but in collapsed patients I typically start with the heart and move towards the abdomen, before returning to assess the lungs – much like the rapid ultrasound for shock and hypotension (RUSH) exam in human medicine.
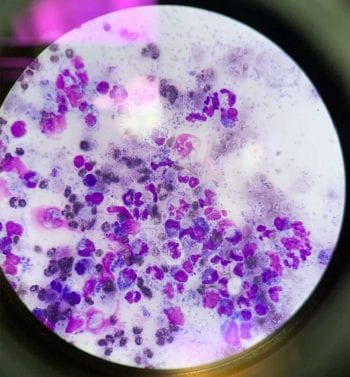
This collapsed patient had a relatively unremarkable thoracic POCUS; however, we were able to identify a small pocket of free fluid in the caudal abdomen, which was safe to aspirate. Abdominocentesis rapidly gave us the answer to this patient’s presentation, and the cytology can be seen in Figure 1.
Bubble was clearly very ill and, unfortunately, after discussion with her owners, they elected to make the difficult decision to have her euthanised.
Everyone deals with euthanasia in different ways. For me, the act of euthanasia isn’t necessarily something that is inherently upsetting. I see euthanasia as a privilege – something that we can do for our patients when their welfare is compromised. It is our duty of care to relieve suffering – even if that means a dignified, humane death.
What I find emotionally difficult is the change of mindset after euthanasia – moving from an intensely emotional situation to the next patient can be challenging, and this is certainly the most difficult part of end-of-life care for me. Trying to approach new cases with a clear mind is important to make sure things don’t get missed, but for me that works best if I can have a few moments to process everything.
Unfortunately, there wasn’t much time to process everything that had happened with Bubble – several patients were waiting. As much as I had only a minor role to play in Bubble’s whole life, it’s a role that is going to be remembered by her owners for a long time. Those last 15 minutes can go very well, or very badly, and that can be a lot of pressure to put on ourselves.
Moving forward
We had around 15 patients come in between 8am and 11am on Monday. Patients were triaged, histories were taken and then we had to decide which to see next.
I would like to think the service we provide at the QMHA is relatively rapid; however, it very much operates like a human accident and emergency clinic – we have to prioritise those patients that are more unstable, or have the potential to become unstable. After a brief chat with our fantastic student group for the day, we came up with a prioritised waiting list and got to work.
Further support came in throughout the day as more interns started their shifts and it allowed us to work through the what seemed to be never-ending patient list. Time quickly ran away with itself and, before I knew it, hour 12 of the shift was fast approaching and I managed to escape to get started on paperwork.
Busy, busy, busy
Over the three days, the hospital saw more than 95 patients through its first opinion emergency service, and more than 20 ECC referrals – it was one of the busiest August bank holidays on record. I think we managed it well and dealt with a few curveballs relatively quickly, but it certainly was tiring.
One of the reasons I love writing these articles is it gives me the chance to reflect on what I’ve done recently. I tend to skim over the previous few articles prior to writing to make sure I don’t repeat myself too much (apologies if I do) and it provides a great opportunity to see how I’m progressing. When I look at my past few articles, it’s really nice to note a gradual improvement in how comfortable I’m feeling.
It’s nice to feel settled in my role as an intern. The hours are long, a lot can be expected of you from a lot of different people, and fairly little free time is available, but I’m loving it. The past few months have been great to see how far I can push myself, and I’m trying my best to be a knowledge sponge – taking in everything that everyone around me has to offer. As I mentioned at this year’s WellVet Weekend, although my working hours are longer and I’m doing a lot more reading in my spare time, I have found this job much less stressful than previous jobs. It’s not for everyone, but I feel like I’m finally back to a place where I can throw myself entirely into the world of veterinary medicine, and I’m just looking forward to seeing where I end up.
That’s all folks!
If you have a question or want to discuss a topic from Practice Makes Perfect, please feel free to drop me an email at dbeeston2@rvc.ac.uk and I will get back to you ASAP. Until next time, take care.
