Introduction
The world is watching the development of new vaccines for SARS-Cov-2 at break-neck speed. One can only marvel at the efforts of scientists, doctors, statisticians and regulators around the world in the race to save us from continued negative impacts on human health and the world economy. However, all of this media coverage has unveiled that so much new technology has been developed in the last two decades that progress towards new medicines is faster than ever.
The development of monoclonal antibody therapies
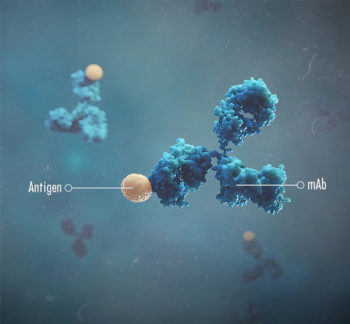
When I was doing my PhD in the Rheumatology Unit at Bristol Royal Infirmary, in the mid-nineties, I remember the excitement of the rheumatologists as they heard of the development of a new mode of therapy for rheumatoid arthritis in the form of a monoclonal antibody against tumour necrosis factor-alpha (TNFα). This pioneering work was performed by Professors Ravinder Maini and Marc Feldmann at the Kennedy Institute in London. Following their ground-breaking laboratory work suggesting a TNF-dependent cascade was at work in inflammatory arthritis, Professors Maini and Feldmann led a proof of principle clinical trial in 1992 using a chimeric anti-human TNFα monoclonal antibody, developed by the US biotech, Centocor. Because anti-human protein antibodies were developed by immunising mice, the antibody must be modified so that it does not evoke an immune response in human patients after repeated injections, so less immunogenic chimeric antibodies have constant regions of human antibodies linked to the variable region of the murine source. Subsequently, the need for even less immunogenicity boosted the production of ‘humanised’ antibodies with only the region that interacts with the antigen epitope being from mouse origin. Nowadays, genetically-engineered mice with genes for a human immune system can be used to produce fully ‘human’ antibodies.
The use of anti-TNFα therapies using antibodies was a major breakthrough, and infliximab (Remicade) was licensed in 1999. Professors Maini and Feldmann quite rightly received knighthoods for their work. Since then, the lives and prognosis of many patients with a variety of inflammatory diseases such as rheumatoid arthritis, ankylosing spondylitis, psoriasis, Crohn’s disease and ulcerative colitis have been changed for the better and other monoclonal antibodies were developed. Interestingly, anti-TNF therapy is now suggested as a potential treatment for COVID-19. TNF is a major component of the cytokine response that is part of the damaging excess inflammatory phase of COVID-19, which is termed hyperinflammation or cytokine release syndrome. Monoclonal antibody therapy is now used for a wide range of conditions including many cancers.
 The expense of monoclonal antibody development and production was such that I thought it would never come to veterinary medicine. However, fast forward a generation and we are now in the midst of the first wave of such treatments for animals. We already have the caninised anti-canine IL-31 antibody, lokivetmab (Cytopoint, Zoetis) which was licensed in 2017 for canine atopic dermatitis, and now we have a new antibody for the management of chronic pain associated with osteoarthritis. This has been realised by incredible advances in technology which have foreshortened the process of producing such therapies. In the past, laborious and time-consuming work would be required to produce a suitable monoclonal by immunising a mouse, creating a hybridoma. There would then be work to identify and modify candidate antibodies. As discussed above, the advance of technology has compressed the process. For veterinary antibody production, one option is to immunize, with adjuvant, a member of the target species with the target molecule to stimulate the production of B lymphocytes producing species-specific antibodies against the target molecule. Peripheral B lymphocytes in blood can then be collected at the peak of the immune response and placed on a single-cell microarray. Lymphocytes producing antibody against the target can be identified and retrieved from the microarray and genes coding for heavy and light chain variable fragments can be amplified and inserted into expression vectors. A mammalian cell line, such as Chinese hamster ovary (CHO) cells, can then be transfected with both the heavy and light chain expression vectors to obtain supernatants containing the whole antibody molecules from where the antibody can be purified. Using this process avoids the need for modification of the antibody since the constant and variable regions are already from the target species.
The expense of monoclonal antibody development and production was such that I thought it would never come to veterinary medicine. However, fast forward a generation and we are now in the midst of the first wave of such treatments for animals. We already have the caninised anti-canine IL-31 antibody, lokivetmab (Cytopoint, Zoetis) which was licensed in 2017 for canine atopic dermatitis, and now we have a new antibody for the management of chronic pain associated with osteoarthritis. This has been realised by incredible advances in technology which have foreshortened the process of producing such therapies. In the past, laborious and time-consuming work would be required to produce a suitable monoclonal by immunising a mouse, creating a hybridoma. There would then be work to identify and modify candidate antibodies. As discussed above, the advance of technology has compressed the process. For veterinary antibody production, one option is to immunize, with adjuvant, a member of the target species with the target molecule to stimulate the production of B lymphocytes producing species-specific antibodies against the target molecule. Peripheral B lymphocytes in blood can then be collected at the peak of the immune response and placed on a single-cell microarray. Lymphocytes producing antibody against the target can be identified and retrieved from the microarray and genes coding for heavy and light chain variable fragments can be amplified and inserted into expression vectors. A mammalian cell line, such as Chinese hamster ovary (CHO) cells, can then be transfected with both the heavy and light chain expression vectors to obtain supernatants containing the whole antibody molecules from where the antibody can be purified. Using this process avoids the need for modification of the antibody since the constant and variable regions are already from the target species.
In an earlier article, I discussed nerve growth factor (NGF) as a central target in synovial joint pain associated with arthritis. Preclinical and clinical research over the last twenty years has clearly demonstrated the important role of NGF in nociceptor sensitisation. NGF is produced and released by peripheral tissues in response to noxious stimuli and when it binds to its main receptor, TrkA, on sensory nerve fibres, the NGF/TrkA complex is internalised and transported to the cell body in the dorsal root ganglia (DRG). This increases the expression of a variety of cell surface receptors and ion channels involved in nociception. This results in an increase the excitability of primary afferent fibres (so-called peripheral sensitisation). NGF/TrkA signalling also leads to the increased expression of pro-nociceptive neurotransmitters such as substance P and calcitonin gene-related peptide (CGRP). Thus, NGF induces functional and phenotypic alterations in the primary afferent fibre.
Preclinical studies in surgically-induced rodent models of OA demonstrated that blocking the action of NGF by using monoclonal antibodies could reduce measured acute and chronic OA pain (McNamee KE and others, 2010; LaBranche and others, 2017; von Loga and others, 2019). This led to the clinical development of anti-NGF antibodies for use in human patients and the results of trials are with the regulators at the time of writing. A recent metanalysis of ten phase III clinical trials human patients with knee or hip OA, one such antibody, tanezumab, can effectively relieve pain and improve physical function and patient’s global assessment in knee and hip osteoarthritis . Thus, based on work in rodent models and human clinical trials, anti-NGF mAb therapy looks promising for the effective control of OA pain. In 2017, tanezumab received FDA fast track designation, recognising the significant potential benefit from this therapeutic.
Development of anti-NGF mAbs for the dog
Canine NGF is closely homogenous to NGF in other species. However, because unmodified monoclonal antibodies from one species can induce an immune response in another species antibodies need to be modified as previously discussed. An anti-NGF monoclonal antibody specifically for canine use was previously developed and underwent clinical trials in dogs with osteoarthritis. In this instance, a rat anti-NGF monoclonal antibody was modified (“caninised”) to allow for use in dogs. This antibody, ranevetmab, indicated a favourable pharmacokinetic profile and no evidence of an acute neutralizing immunogenic response in dogs. Two published clinical trials evaluated the efficacy of single intravenous injection of ranevetmab in to dogs with osteoarthritis. In a randomised and double-blind study where all dogs received ranevetmab, the safety and clinical effect was examined using an owner completed questionnaire—the Canine Brief Pain Inventory (CBPI) score (Webster and others, 2014). Nine dogs with OA received a single injection of ranevetmab during the 10 weeks of study period (either at the start, two or four weeks into the study), with owners blinded to the time of injection. This study showed that significantly lower CBPI scores were seen compared with baseline scores until four weeks after treatment, and although values were not statistically significant, CBPI scores at six weeks after administration were still lower than baseline scores. In another randomised, double-blind, placebo-controlled trial, 26 dogs suffering from OA pain were allocated to placebo or treatment group based on predominant site of problem and CBPI score (Lascelles and others, 2015). The dogs were assessed every two weeks for four weeks owner-completed clinical metrology instruments (CBPI, Client-Specific Outcome Measures (CSOM) and Liverpool Osteoarthritis in Dogs) for the evaluation of efficacy. The dogs that received ranevetmab had significant improvement in all three CMIs compared with baseline scores throughout the study period. In both clinical studies, no adverse events associated with treatment were reported. Renevetmab was developed by a company called Nexvet Biopharma plc which was purchased by Zoetis Inc. in 2017.
In September 2020, the European Medicine Agency Administration adopted a positive opinion of the anti-NGF monoclonal antibody bedinvetmab (Librela, Zoetis) for “the alleviation of pain associated with osteoarthritis in dogs”. At the recommended dose once a month, bedinvetmab resulted in clinically relevant improvements in owner assessment scores of pain severity, pain interference and life quality in dogs with osteoarthritis. The agency state that bedinvetmab (Librela) is generally well tolerated at the recommended dose; mild reactions at the injection site (e.g. swelling and heat) may uncommonly be observed
Summary
 NGF is a key mediator in chronic pain in osteoarthritis with a compelling body of laboratory, pre-clinical and clinical evidence regarding its pivotal role. Blocking the action of NGF in the osteoarthritic joint has great potential to improve the lives of affected pets and, consequently, their owners. After a generation of work to understand the actions of NGF and how to control it, in parallel with all the breakthroughs in monoclonal antibody development, we now have the first monoclonal antibody therapy for canine osteoarthritis. The requirement for a once monthly injection also likely brings the management of osteoarthritis more under the supervision of the veterinary team. I think this will be positive in terms of holistic management of the disorder and will raise the quality of veterinary care for affected dogs. This could be a real paradigm shift in managing this challenging and lifelong condition.
NGF is a key mediator in chronic pain in osteoarthritis with a compelling body of laboratory, pre-clinical and clinical evidence regarding its pivotal role. Blocking the action of NGF in the osteoarthritic joint has great potential to improve the lives of affected pets and, consequently, their owners. After a generation of work to understand the actions of NGF and how to control it, in parallel with all the breakthroughs in monoclonal antibody development, we now have the first monoclonal antibody therapy for canine osteoarthritis. The requirement for a once monthly injection also likely brings the management of osteoarthritis more under the supervision of the veterinary team. I think this will be positive in terms of holistic management of the disorder and will raise the quality of veterinary care for affected dogs. This could be a real paradigm shift in managing this challenging and lifelong condition.
References and further reading
- McNamee KE, Burleigh A, Gompels LL, Feldmann M, Allen SJ, Williams RO, Dawbarn, D, Vincent TL, Inglis JJ (2010). Treatment of murine osteoarthritis with TrkAd5 reveals a pivotal role for nerve growth factor in non-inflammatory joint pain, Pain 149: 386–392.
- LaBranche TP, Bendele AM, Omura BC (2017). Nerve growth factor inhibition with tanezumab influences weight-bearing and subsequent cartilage damage in the rat medial meniscal tear model, Annals of the Rheumatic Diseases 76: 295–302.
- von Loga IS, El-Turabi A, Jostins L. (2019). Active immunisation targeting nerve growth factor attenuates chronic pain behaviour in murine osteoarthritis, Annals of the Rheumatic Diseases 78: 672–675.
- Fan ZR, Ma JX, Wang Y, Chen HT, Lang S, Ma XL (2020). Efficacy and safety of tanezumab administered as a fixed dosing regimen in patients with knee or hip osteoarthritis: a meta-analysis of randomized controlled phase III trials, Clinical Rheumatology DOI: 10.1007/s10067-020-05488-4
- Enomoto M, Mantyh PW, Murrell J, Innes JF, Lascelles BDX (2019). Anti-nerve growth factor monoclonal antibodies for the control of pain in dogs and cats, Veterinary Record 184, 23.
- Lascelles BDX, Knazovicky D, Case B, Freire M, Innes JF, Drew AC, and Gearing DP (2015). A Canine-Specific Anti-Nerve Growth Factor Antibody Alleviates Pain and Improves Mobility and Function in Dogs with Degenerative Joint Disease-Associated Pain, BMC Veterinary Research 11: 101
- Webster RP, Anderson GI, Gearing DP (2014). Canine brief pain inventory scores for dogs with osteoarthritis before and after administration of a monoclonal antibody against nerve growth factor, American Journal of Veterinary Research 75: 532–5.
Librela contains bedinvetmab POM-V. For the alleviation of pain associated with osteoarthritis in dogs.
For further information please see the product’s SPC or contact Zoetis UK Ltd, First floor Birchwood Building, Springfield Dr, Leatherhead, KT22 7LP www.zoetis.co.uk Customer Support: 0845 300 8034 or customersupportUK@zoetis.com Use medicines responsibly (www.noah.co.uk/responsible) Date of preparation: April 2021. MM-14021

Leave a Reply