Have you ever stopped to consider how you came to decide what a normal body temperature is for your patients? Or noticed that what you would consider to be a temperature in the pyrexic range is different to that of your colleagues?
How can you be certain that your interpretation of a body temperature measurement in a dog or cat is accurate for that particular individual?
You may be surprised to know that what most veterinary professionals may consider as a normal reference range for body temperature is based on little robust evidence-based veterinary literature1!
In fact, normal body temperature is poorly defined in veterinary literature. The expectation for a reference range is that a suitably large population has been used with a robust statistical analysis performed to determine a “normal” range, with 95% of that population sitting within it. The reality is that reference ranges stated in textbooks often fail to state their primary source, which makes it impossible to know the size or demographics of the population used, or whether the range was statistically calculated1 (Table 1).
| Normal reference intervals in cats | Publications |
|---|---|
| 37.8°C-39.2°C | Khan CM and Line S (2010). The Merck Veterinary Manual, Merck and Co, White House station: 2,822.
Smith VA, Lamb V and McBrearty AR (2015). Comparison of axillary, tympanic membrane and rectal temperature measurement in cats, Journal of Feline Medicine and Surgery 17(12): 1,028-1,034. |
| 37.8°C-38.9°C | Hartman K and Levy JK (2011). Feline Infectious Diseases, Manson publishing, London: 215. |
| 37.2°C-39.2°C | Shojai AD (2001). The First Aid Companion for Dogs and Cats. Emmaus, Rodal, Emmaus: 248. |
| 38°C-38.5°C | Lane DR and Guthrie S (2004). Dictionary of Veterinary Nursing (2nd edn), Elsevier, Edinburgh: 201. |
| 38.1°C-39.2°C | Frederichs K, Barnhart K, Blanco J et al (2008). Guidelines for the determination of reference intervals in veterinary species and other related topics, Clinical and Laboratory Standards Institute, Wayne. |
Based on this, how can we be sure that the reference range quoted is accurate or applicable to the patient in front of us?
Does a normal temperature exist?
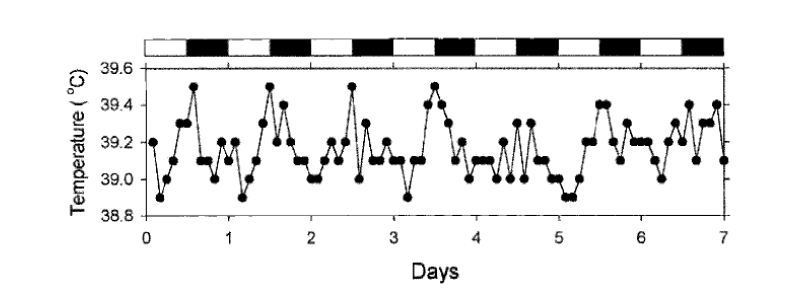
In addition, body temperature is not constant. Body temperature, in common with most essential physiological functions such as heart and respiration rate, blood pressure, sleep/wake cycle etc., also follows a circadian rhythm. A 2003 study8 demonstrated this for the first time in seven female beagle dogs, where rectal temperature was measured every 2 hours for 1 week under rigorously controlled conditions (ambient temperature, lighting, exercise and diet).
Interestingly the mean rectal temperature in this study was 39.1°C, which is 0.2°C above the body temperature (38.9°C) generally considered “normal” in dogs.
The data from all seven dogs supported the same conclusions: body temperature started to increase immediately after feeding and lasted until lights-out, 8 hours later (Figure 1). Feeding was not the cause of the day-long increase in body temperature. Given that the environmental conditions were strictly controlled the only cause for the change was endogenous.
Individual physiological factors also contribute to variation in an individual’s body temperature and include breed9, age9, sex9,10, body condition9, level of activity11 and stress levels12.
Given the level of individual variation surely it would make sense to get an understanding of an individual pet’s temperature range in order to interpret body temperature measurements accurately?
“Gold standard” temperature monitoring
To measure true core temperature either blood temperature, urinary bladder temperature or oesophageal temperature must be measured. However, these methods are invasive and impossible to utilise in the conscious patient.
Rectal thermometry remains the “gold standard” for temperature measurement based on its good correlation with core body temperature2 and familiarity within the veterinary profession, however this method isn’t without its drawbacks or inaccuracies. It can be stressful and not always well tolerated in conscious animals3-5. Rectal temperature measurements can be affected by faecal material, rectal inflammation, thrombotic conditions6, peristalsis, muscle tone, physical activity2, and even just by having the thermometer inserted at an insufficient depth. It can also be the cause of cross-contamination of rectal bacterial flora7 between patients.
An alternative method avoiding the drawbacks mentioned above is available – and it is as simple as reading a microchip, especially if that chip is a HomeAgain® Thermochip®.
HomeAgain® Thermochip® is a microchip with a difference, as it has an integrated temperature biosensor. Obtaining a temperature reading is as easy as scanning the microchip with a compatible scanner, such as the SureSense® Universal microchip reader or the Global Pocket Reader® Plus. As the temperature is measured in the subcutaneous space (where the microchip is implanted) it does not read the same temperature as a rectal thermometer – so these two methods cannot be directly compared. However, given this method is easier, less invasive and can be performed repeatedly it is simple method to ascertain an individual’s temperature reference range.
Reliability and accuracy
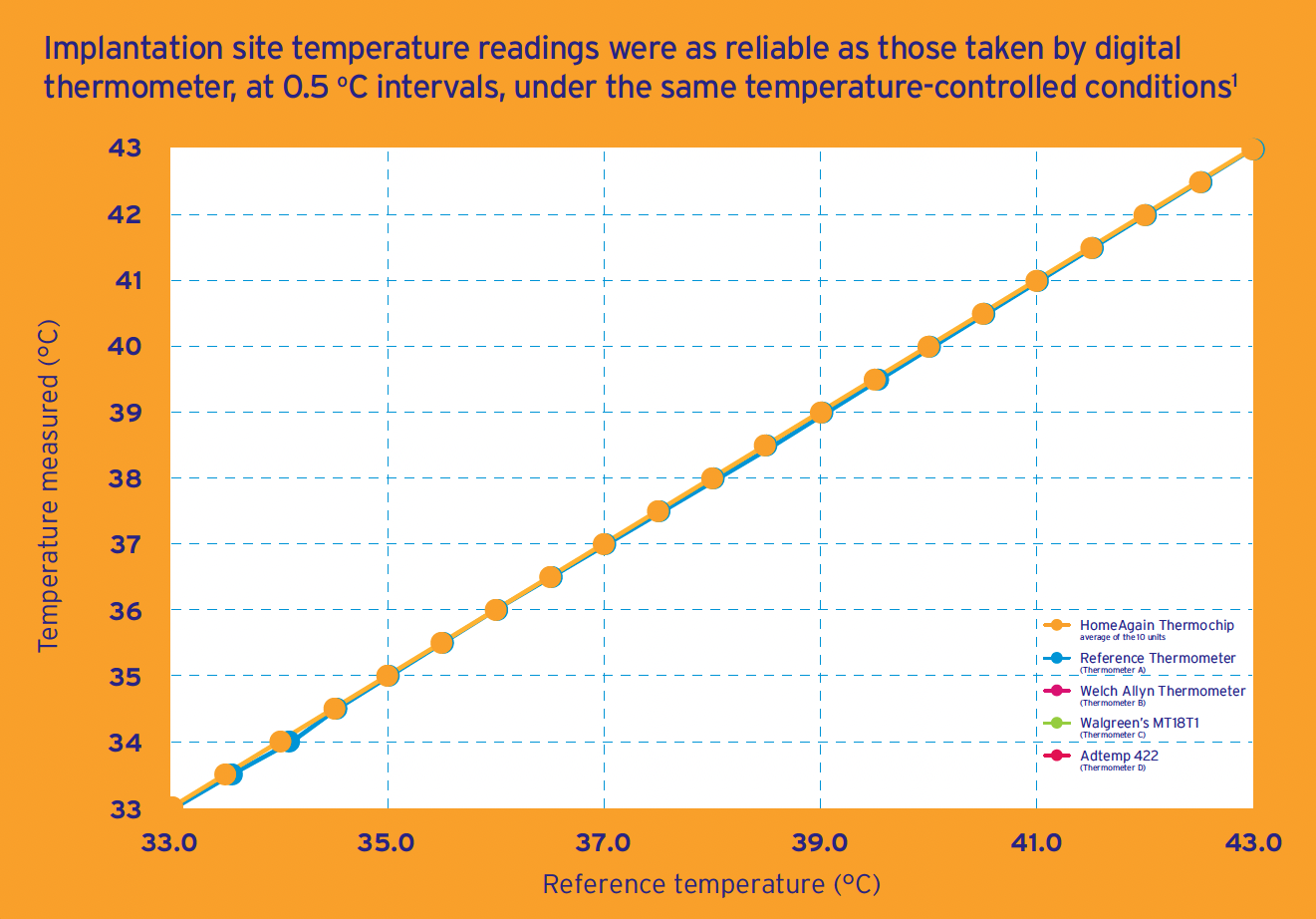
The HomeAgain® Thermochip® microchip is just as reliable and accurate as your trusty digital rectal thermometer, as an independent laboratory study demonstrated13. This study compared the temperature readings of 10 HomeAgain® Thermochip® microchips with 4 digital thermometers placed in the same temperature-controlled conditions between 33°C and 43°C at 0.5°C intervals and confirmed the reliability and accuracy of HomeAgain® Thermochip® (Figure 2).
The ability to detect a fever is an important factor when considering a different method of recording temperature, and the HomeAgain® Thermochip® is very capable of picking this up.
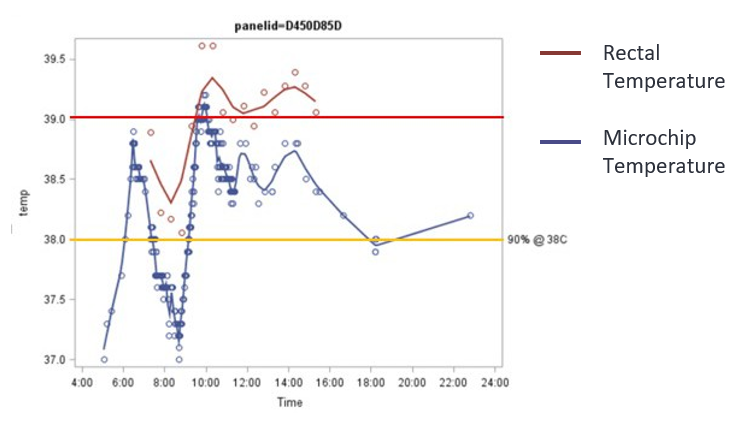
In an unpublished study HomeAgain® Thermochip® was able to detect the same physiological fever patterns as rectal thermometry. In this study14 10 Beagle dogs were given an intravenous injection of lipopolysaccharide and their temperatures were monitored 4 to 8 hours after the injection to record the febrile response. Rectal temperatures were taken every 30 minutes and the HomeAgain Thermochip was scanned every 5 minutes.
Following fever induction, 2,721 temperatures were collected from the 10 dogs, with the greater majority measured using HomeAgain Thermochip. The challenge response was unique for all dogs but was characterised by an initial decrease in temperature (vasoconstriction) followed by a gradual increase to peak temperature demonstrated by both rectal and HomeAgain Thermochip temperature monitoring following a similar shaped curve (Figure 3).
Clinical applications and the future of temperature monitoring
Although our reliance on rectal thermometry will not be disappearing anytime soon having an alternative temperature recording method which is reliable, accurate, easy, non-invasive and doesn’t distress the patient may encourage us to change our established routines. Especially if this method allows us to obtain an individual pet’s reference range from which we can interpret temperature variations correctly.
The HomeAgain® Thermochip® microchip can already be used for various clinical applications, including as a screening tool or as part of the clinical examination, monitoring temperature during anaesthesia, surgery and the post-operative period, or for hospitalised patients, particularly those that need regular temperature monitoring.
But what does the future look like?
Popular pet-tech consumer brand, Sure Petcare, has the ability to collect temperature data from pets implanted with temperature-sensing microchips with their connected feeder and fountain products. There are currently thousands of pets using these connected devices today and these have collected millions of temperature measurements, with numbers continuing to grow!
So, if you want your clients, their pets and yourself to benefit from the additional information that a HomeAgain® Thermochip® can contribute to the health data from this connected ecosystem then recommend a HomeAgain Thermochip today!

Leave a Reply