Gastrointestinal conditions are commonly presented in practice yet can still be very difficult to manage in a standard consultation. Not only is there a long list of potential differentials, history taking can also be time consuming and obtaining the owner’s cooperation and confidence can be key to managing the condition moving forwards.
Adopting a structured approach is one way to improve concordance with your dietary recommendation.
This article will describe and apply this structured approach and also signpost to a variety of resources such as video, podcasts and tools to help with the communication and engagement with the pet owner.
Towards collaborative care
Each case involving a nutritional recommendation requires five basic steps to take place:
- Nutritional assessment
- Nutritional recommendation
- Plans for follow up
- Record the outcomes
- Reassess each visit
The Purina Institute’s CentreSquare resource offers tools and tips across all of these areas, including useful guides for pet owners to provide support beyond the consultation room. The aim is to create a programme of collaborative care – so the owner understands the choices available to them and the impact those choices might have on their pet’s health and welfare.
Acute or Chronic?
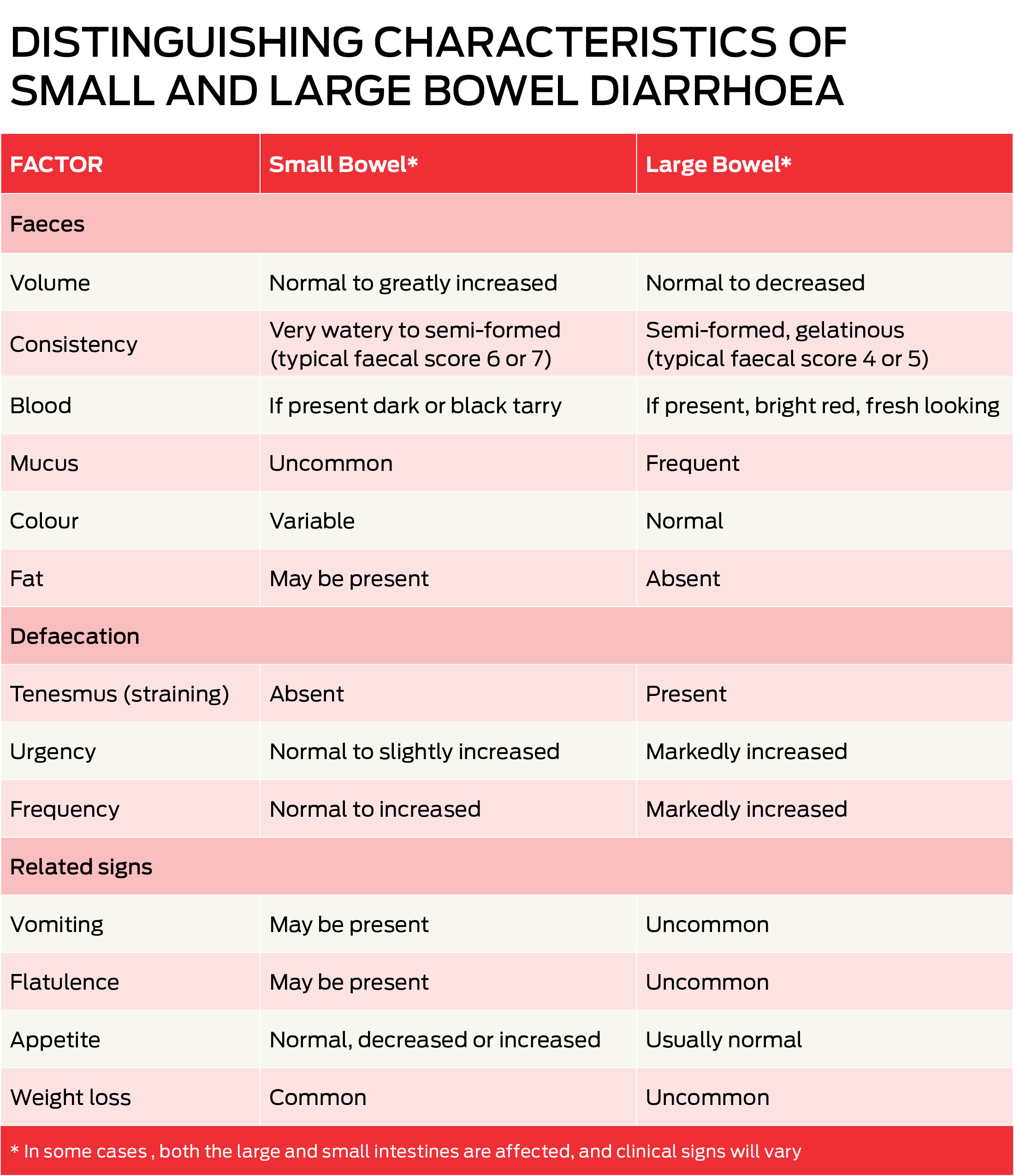
While the basic framework of how they are approached stays the same, acute and chronic GI conditions may warrant a very different management strategy. Nutritional management is also likely to vary depending on whether the small or large bowel is mainly affected.
Structured conversations
The majority of pet owners (90%) want to receive a nutritional recommendation from their vet but less than 15% actually receive one.1 Some discussions on nutrition can be difficult or even emotional.
An initial conversation starter can be used to engage the owner and addressing the main key messages ensures an accurate and compelling recommendation is made. We’ll look at two scenarios as examples in this article: conversations around feline acute gastroenteropathy and canine chronic enteropathy.
- Conversation starter
- What to feed
- When to feed
- How to feed
Did you know?
- Food form (eg, liquid, canned, or dry) influences how quickly the stomach empties. Liquid diets are the fastest to leave the stomach, followed by canned foods and finally dry kibble.
- The increased moisture content of a wet formula or warm water added to dry food can help offset mild fluid losses while improving palatability.
- Small, frequent meals (e.g., 3 to 6 meals per day) can help improve nutrient absorption and minimise adverse responses such as vomiting or diarrhoea.2.3
Structured approach to feline acute gastroenteropathy in action
In the absence of confirmation of inflammation, gastroenteropathy is the starting point. Presentation may include vomiting, diarrhoea, or disrupted food intake. This may be due to infections, dietary indiscretion, hairballs, or intolerance, or secondary to systemic disease. While signs may resolve spontaneously, severe or prolonged cases often require identification of the underlying disease.
 The goals of nutritional management of cats with acute gastroenteropathy are to provide a diet that meets the cat’s nutrient requirements, minimises irritation to the GI mucosa, reduces GI secretions, supports normal motility of the stomach and intestines, and reduces risk for gastroesophageal reflux and vomiting.
The goals of nutritional management of cats with acute gastroenteropathy are to provide a diet that meets the cat’s nutrient requirements, minimises irritation to the GI mucosa, reduces GI secretions, supports normal motility of the stomach and intestines, and reduces risk for gastroesophageal reflux and vomiting.
Conversation starter
“Vomiting or diarrhoea can be unpleasant and stressful for both you and your cat, and we want your pet to feel better as quickly as possible. Your cat’s GI tract may need a little time to heal, even after the signs resolve. Feeding a highly digestible diet during recovery can help get your cat back to normal as quickly as possible. After that, we can plan to transition back to your pet’s regular diet.”
What to feed – nutritional approaches to consider
Withholding food for a short period (12-24 hours) is a standard recommendation for cats with acute, non-life-threatening gastroenteropathy. This will help to reduce severity and frequency of vomiting, reduce risk of aspiration pneumonia, minimise additional fluid losses, and decrease discomfort.
Prolonged (>48 hours) fasting should be avoided because it can contribute to atrophy of the intestinal mucosa, delayed recovery of intestinal function, and development of malnutrition or problems such as dysbiosis or hepatic lipidosis in obese cats.
When to feed – dietary characteristics and interventions
Fluid intake: Cats with mild fluid deficits that are not vomiting can be managed with oral water intake or subcutaneous fluid administration. Cases of moderate to severe dehydration should receive intravenous fluid and electrolyte replacement.
Vomiting may require therapeutic management, and as it resolves and electrolyte balance is restored, small amounts of water can be offered every few hours. Fluid intake should be monitored to ensure adequate consumption.
Digestibility: a palatable, easily digestible, higher-protein formula is appropriate for cats and early enteral feeding is encouraged. In contrast to dogs, dietary fat does not slow gastric emptying in cats, so a fat-restricted diet is typically not needed when managing cats with GI signs.
How to feed – feeding management
- An initial feeding target of 25% to 33% of resting energy requirement (RER) calories, divided into 3 to 6 meals per day, may optimise recovery of the intestinal mucosa
- If the cat can eat small amounts of food without episodes of vomiting or diarrhoea, the amount fed can be increased, and frequency per day decreased, over several days until the pet returns to its normal eating schedule.
- If the gastroenteropathy has resolved, a gradual transition to the normal diet can be undertaken over a 5-7 day period.
Find out more about managing acute GI conditions here:
Structured approach to chronic enteropathy in dogs in action
Dogs with chronic enteropathy may have a combination of gastrointestinal signs of varying severity, including chronic intermittent or persistent diarrhoea and/or vomiting, weight loss, changes in appetite, borborygmus, nausea, and abdominal pain.
Key characteristics
- Non-specific
- Clinical signs lasting three weeks or longer
- Other causes (e.g. parasites, bacterial infections, cancer, and non-GI diseases) have been excluded 4-7
- One or more segments of the GI tract are affected 4,8,9
Chronic enteropathy can be grouped into four categories based on treatment response, intestinal biopsies and histopathology, or both: 10
- food-responsive enteropathy
- antibiotic-responsive enteropathy
- immunosuppressant-responsive enteropathy (includes steroid-responsive enteropathy and inflammatory bowel disease)
- non-responsive enteropathy
Dietary intervention may be used for both diagnosis and therapeutic management of dogs with chronic enteropathy. Many dogs respond well to dietary changes that eliminate adverse reactions to food. An elimination diet trial is now frequently recommended before endoscopy for most dogs with chronic GI signs of mild to moderate severity for which no other causes are identified and there are no contraindications (e.g. hypoalbuminemia, hypocobalaminemia).4, 5, 11-14
Conversation starter
“Your dog has a gastrointestinal disease known as chronic enteropathy and there are different types of this condition. I think [dog’s name] may benefit from a change in food, and I am recommending we start [him/her] on a therapeutic diet that is designed for this condition. We should see improvement within two weeks and, if not, we can discuss trying a different food or next steps.”
What to feed – nutritional approaches to consider
There is no one size fits all approach for dogs with chronic enteropathy. Common dietary strategies may include:15-20
- Highly digestible, low-residue/low fibre diets
- Novel protein/hydrolysed diets
- Low-fat diets
- Fibre-enriched diets
Initial selection of a highly digestible, commercial therapeutic gastrointestinal diet has been supported by studies.18 For those dogs that do not respond but remain stable clinically, an elimination diet should be used. A response should be seen within 1-2 weeks. Failure to respond to the second trial may indicate further diagnostics such as an antibiotic trial or intestinal biopsy.
When to feed – dietary characteristics and interventions
Digestibility: Important when the ability of the GI tract to digest food and absorb nutrients, particularly protein and fat, may be compromised. High digestibility helps improve nutrient absorption and minimise complications associated with undigested food (e.g., osmotic diarrhoea or altered colonic microbiota).
Protein: High digestibility helps dogs with compromised digestive function absorb sufficient essential amino acids. Noteworthy if adverse food reactions are suspected.
Energy density: An energy-dense diet can help reduce meal size which is important for dogs with reduced appetite and/or decreased digestive function21. High energy density diets are usually higher fat, and this may need to be restricted if pancreatitis or lymphangiectasia is present. Replacing some of the fat with medium chain triglycerides may be beneficial.
An increased amount of fat in the colon may induce dysbiosis, epithelial cell damage, and fluid secretion into the colon. This is a consideration where fat digestion and absorption are compromised. Omega-3 to omega-6 fatty acids may modulate intestinal inflammation by reducing production of proinflammatory metabolites.
Fibre: Low-fibre is traditionally recommended to avoid delayed gastric emptying and to improve nutrient absorption in small bowel diarrhoea and vomiting. In large bowel diarrhoea, a high-fibre diet containing soluble and insoluble fibre may help reduce tenesmus and assist mucosal repair in the colon.
Probiotics: Especially those shown to modulate the immune system or to have anti-inflammatory properties. Probiotics may benefit some dogs with chronic enteropathy as part of a multimodal therapeutic approach.22
How to feed – feeding management
- Small, frequent meals recommended
- Gradual transition to the dog’s usual diet over a 7-day period may be possible.
- Some dogs may need to remain on a therapeutic diet.
Find an update on nutritional strategies for chronic GI conditions here:
Access a free ebook on the role of the microbiome in GI function here:
Related tools
For veterinary teams:
To share with owners:




Leave a Reply