Anything that causes narrowing or obstruction of the airways may be associated with reduced performance – particularly in elite athletes.
Disorders of the upper respiratory tract are often accompanied by respiratory noise that affects a horse’s value, even if it does not adversely affect performance. Some historic and physical examination features may point to a specific condition; however, resting and exercising endoscopy are often necessary to obtain definitive diagnosis.
Increasing use of exercising endoscopy has revealed multiple airway abnormalities often coexist, and the findings of sequential examinations of the same horse can differ (McGivney et al, 2019).
Diagnostics
History
As ever, accurate history taking is crucial. Important points to ascertain include signalment, onset and duration of signs, presence of respiratory noise, perceived performance issues and the presence of coughing or nasal discharge.
Specific features of poor performance or respiratory noise may be suggestive of the diagnosis. For example, abrupt decline in performance and a “gurgling” expiratory noise may be indicative of dorsal displacement of the soft palate (DDSP), whereas an inspiratory “whistle” and gradual decline in performance is more likely to be associated with recurrent laryngeal neuropathy (RLN) or other causes of dynamic inspiratory collapse.
Despite these apparent associations, limitations of using sound to make diagnoses are evident (Cable et al, 2002; Cramp et al, 2009), so audible clues must not be relied on. Use of respiratory noise alone is likely to result in incorrect diagnosis in approximately 50% of cases (Witte et al, 2011).
Reports of increased respiratory effort at rest, protracted recovery from exercise, the presence of a cough or bilateral nasal discharge are all suggestive of disease of the lower respiratory tract (LRT).
Physical examination
General physical examination, including cardiothoracic auscultation, should not be overlooked – even if an upper respiratory tract (URT) condition is suspected – as LRT disorders may cause or contribute to URT dysfunction and laryngeal disorders may result in lower airway disease.
Thoracic auscultation has low sensitivity for identifying equine asthma, so lower airway endoscopy and collection of lower airway washes should always be considered. Laryngeal palpation should be employed in cases presenting with suspected URT dysfunction.
Laryngeal asymmetry should be noted – for example, cricoarytenoideus dorsalis muscle (CAD) atrophy may be palpable as a more prominent muscular process on the affected (left) side. Careful palpation may identify a space between the thyroid and cricoid cartilage, suggestive of laryngeal dysplasia (Garret et al, 2009).
Endoscopy
Resting endoscopy is readily available, and remains an important diagnostic tool for evaluation of the larynx, pharynx and lower airways. Chemical restraint should be postponed until the URT has been examined, given its effects on upper airway function.
Examination via the right ventral meatus may be preferable versus the left to avoid artifactual changes in left arytenoid position and movement (Smith and Dixon, 2015). URT anatomy should be assessed, and a careful examination performed for evidence of previous URT surgery.
Although logical that poor arytenoid function at rest would be associated with compromised function during exercise, in reality, resting endoscopic examination may be poorly reflective of dynamic function at high speeds (Kelly et al, 2013).
Exercising endoscopy is, therefore, valuable and can be performed during exercise on a treadmill (high speed treadmill endoscopy) or overground. Overground endoscopy (OGE; Figure 1) is generally preferred as it replicates the normal training regimen and head position (Franklin et al, 2006; Pollock et al, 2009).

Definitive diagnosis of dynamic respiratory obstructions and complex airway abnormalities is heavily reliant on exercising endoscopy. For those cases managed surgically, postoperative exercising examinations allow for more critical evaluation of outcome. Previously, performance and respiratory noise would have been used to evaluate outcome; however, neither are reliable (Brown et al, 2004; Pollock, 2017).
The quantity of mucus in the trachea is assessed endoscopically and a subjective grade applied (Table 1). Due to the efficiency of the mucociliary escalator in normal horses, little or no mucus should be present in a healthy respiratory tract.
| Table 1. Grading system for trachea mucus | |
|---|---|
| Grade | Description |
| 0 | No mucus |
| 1 | Multiple small blobs of mucus |
| 2 | Large blobs of mucus |
| 3 | Streams of mucus |
| 4 | Pooling mucus |
| 5 | Extreme/profuse mucus pooling ventrally with blobs dorsolaterally |
| (Gerber et al, 2004) | |
Tracheal aspirate
Tracheal aspirates may be collected via trans-endoscopic and trans-tracheal methods. A trans-tracheal aspirate is not performed commonly in the UK and is indicated where a sterile sample needs to be obtained – for example, in cases of pleuropneumonia.
However, it is invasive and carries a risk of infection at the incision site, so is less commonly performed – especially when good transendoscopic technique minimises the risk of sample contamination (Christley et al, 1999).
A trans-endoscopic tracheal aspirate allows visualisation of the airways and grading of the mucus present (Allen and Franklin, 2010). It is essential the tip of the endoscope remains proximal to the fluid pool prior to sampling to prevent contamination with oropharyngeal bacteria.
Bronchoalveolar lavage
Bronchoalveolar lavage (BAL) is considered the most sensitive and specific diagnostic test for equine asthma (Cian et al, 2015; Mazan, 2018). While tracheal wash (TW) samples also provide cytological evidence of airway inflammation and increased mucus production, the results are not reliably reflective of lower airway pathology.
Evidence supports a correlation between cough and TW neutrophilia; however, correlation remains poor between the cytological appearance of TW and BAL fluid (BALF) samples from the same horse, as well as between poor performance and TW cytology.
As such, cytological examination of BALF is the recommended approach to investigation of equine asthma in practice, and is not equivalent to cytological examination of TW samples (Couëtil et al, 2016).
To obtain a sample of BALF, horses should be sedated appropriately (the authors use approximately 0.01mg/kg detomidine and 0.01mg/kg butorphanol IV); the use of butorphanol in the sedative regimen has the added value of an antitussive effect.
A solution of local anaesthetic and saline (LAS) should be prepared, with 15ml lidocaine in 15ml saline. The BAL tube is passed via the ventral nasal meatus and, with the head and neck extended, passed through the rima glottidis into the trachea.
Once in the proximal trachea, approximately 10ml of LAS is instilled before the tube is further advanced to the approximate level of the thoracic inlet, at which point the remaining LAS is instilled and followed with air to clear the tube.
The tube is then further advanced until it becomes wedged, at which point the cuff can be inflated. Other techniques can be used, depending on the operators’ preference, including endoscopically guided BAL, which enables sampling from a specific region. Application of a twitch may make the horse more amenable to the procedure.
The volume to be instilled varies between 250ml to 500ml 0.9% saline, depending on personal preferences. However, the authors routinely use 300ml (5 × 60ml syringes), instilled as 2 syringes injected, then withdrawn to retrieve as much sample as possible (with minimal withdrawal force to reduce airway collapse), followed by 3 syringes injected, then withdrawn to retrieve the remainder of the sample, with approximately 50% to 70% return of infused fluid expected.
The sample is then pooled, and an aliquot collected and submitted in ethylenediamine tetra-acetic acid for cytological evaluation.
If cytological evaluation is delayed, the sample should be fixed by addition of an equal volume of 10% buffered formalin or ethanol (40%) at the time of collection (Cian et al, 2015). This is important, as leukocytes will continue to phagocytose free bacteria within the sample, giving a false indication of intracellular bacteria and cellular degeneration within an unfixed sample.
Cellular preservation rapidly becomes poor, reducing the validity of subsequent cell counts. Prompt evaluation of samples is important to ensure accurate results.
Ultrasonography
Laryngeal ultrasonography is a useful adjunctive diagnostic technique for URT disorders (Garrett, 2015). Several ultrasonographic “windows” are described laterally and ventrally (Chalmers at al, 2006; (Figure 2).

Once familiar with the normal anatomy, laryngeal ultrasound provides useful information in a cost-effective and noninvasive manner – particularly relevant to recurrent laryngeal neuropathy, arytenoid chondritis and fourth branchial arch defects (Garrett, 2018).
Ultrasonographic examination of the LRT is unlikely to be rewarding in horses with mild, performance-limiting disease.
Radiography
Although interpretation of head radiographs can be difficult, some useful information can be gained – particularly with respect to the subepiglottic region.
Radiographs may also be useful in the assessment of laryngeal position before and after performing a laryngeal tie forward procedure, to confirm the larynx has been fixed in a more rostral position and help determine implant failure in cases where palate displacement persists postoperatively (Woodie et al, 2005).
It is unlikely radiographic abnormalities of the LRT would be present in horses with mild, performance-limiting disease and it would not typically be performed.
RLN
RLN is a bilateral mononeuropathy of the recurrent laryngeal nerves, with unilateral left CAD muscle atrophy predominating, resulting in varying degrees of left arytenoid paralysis and ipsilateral vocal fold collapse.
During resting endoscopy, numerous grading scales have been used to describe laryngeal position and function, with the Havemeyer grading scale being the most widely employed (Dixon et al, 2004; Table 2).
| Table 2. Havemeyer scale of laryngeal function | ||
|---|---|---|
| Grade | Description | Subgrade |
| 1 | All arytenoid movements are synchronous and symmetrical. Full arytenoid abduction achieved and maintained | |
| 2 | Arytenoid movements are asynchronous and/or asymmetrical at times, but full arytenoid abduction is achieved and maintained | .1 transient asynchrony, flutter or delayed movements are seen |
| .2 asymmetry of the rima glottidis much of the time due to reduced mobility of the arytenoid, but occasions exist, typically after swallowing or nasal occlusion, where full symmetrical abduction is achieved and maintained | ||
| 3 | Arytenoid movements are asynchronous and/or asymmetrical at times. Full arytenoid abduction cannot be achieved and maintained | .1 asymmetry of the rima glottidis much of the time due to reduced mobility of the arytenoid, but occasions exist, typically after swallowing or nasal occlusion, where full symmetrical abduction is achieved, but not maintained |
| .2 obvious arytenoid abductor deficit and asymmetry. Full abduction is never achieved | ||
| .3 marked, but not total arytenoid abductor deficit and asymmetry. Full abduction is never achieved | ||
| 4 | Complete immobility of the arytenoid cartilage and vocal fold | |
| (Dixon, 2004) | ||
Although the majority of horses with resting laryngeal grades 1 and 2 are able to fully abduct both arytenoid cartilages during exercise, and those with resting grades 3 and 4 are much more likely to experience dynamic laryngeal collapse, it is increasingly recognised resting endoscopy is not always reflective of the dynamic situation.
For example, horses with “normal” resting laryngeal grades may experience laryngeal collapse during exercise and those with “abnormal” resting laryngeal grades may be able to achieve full abduction at speed. For accurate diagnosis of dynamic laryngeal function (or dysfunction), exercising endoscopy remains the gold standard. Laryngeal function may also be graded at exercise (Figure 3).
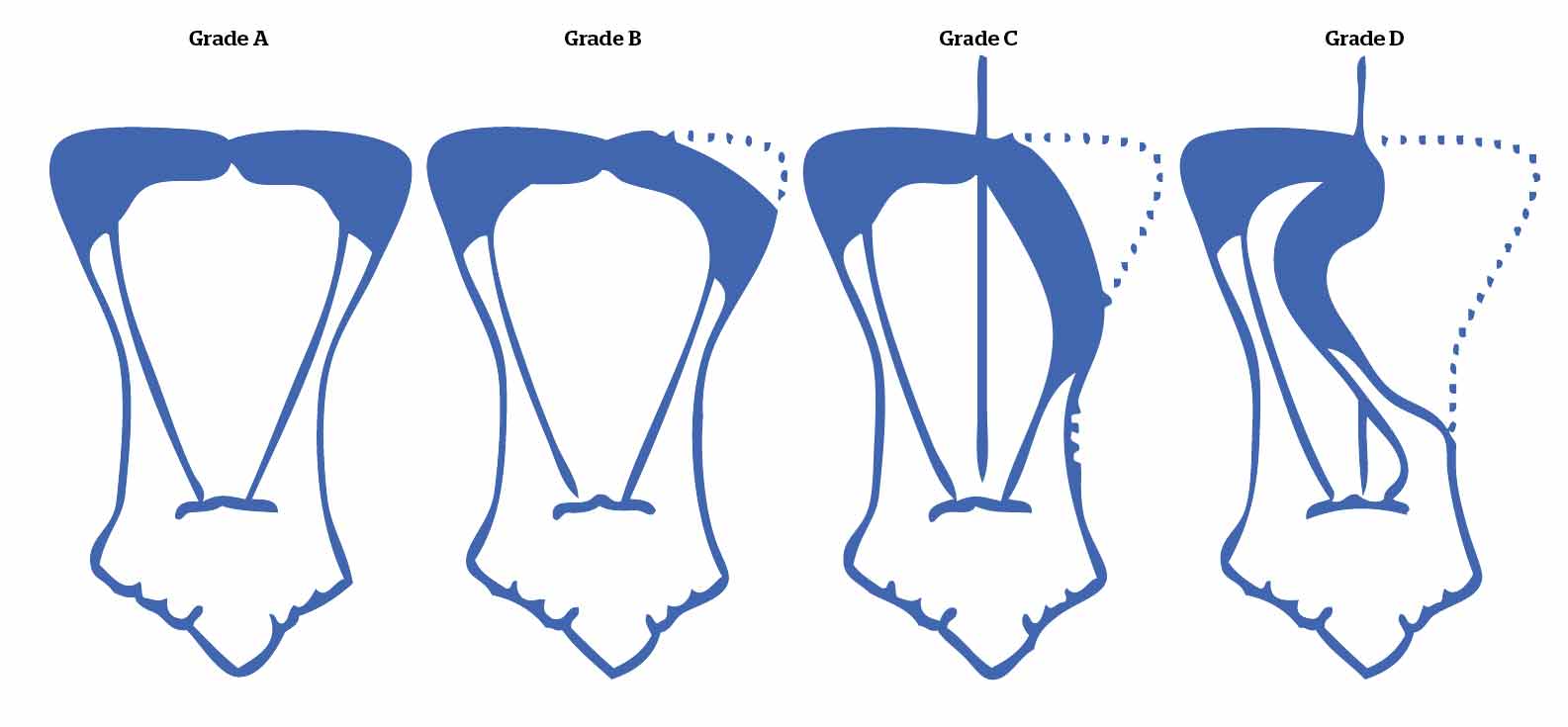
Management of RLN depends on the use of the horse and severity of arytenoid cartilage collapse, but for those expected to perform at maximal intensity (that is, racehorses), surgical intervention is likely to be required, with numerous options available.
Prosthetic laryngoplasty (“tieback”) was described in the 1970s (Marks et al, 1970), and has since become one of the most commonly applied surgical treatments for affected horses around the world – especially for those horses with grade 4 laryngeal function.
However, a wide range of success rates have been reported in different populations; 70% to 90% return to racing (Goulden et al, 1982; Strand et al, 2000; Dixon et al, 2003; Barakzai et al, 2009a), and modest-at-best success in high level athletes, with 78% of horses treated with laryngoplasty experiencing dynamic airway collapse during OGE in one study (Barnett et al, 2013b).
The procedure is also not without its complications, including loss of arytenoid abduction, dysphagia, persistent coughing and airway contamination, to name a few. Postoperative abduction grading is described in Table 3.
| Table 1. Grading of laryngeal abduction following prosthetic laryngoplasty | |
|---|---|
| Grade | Description |
| 1 | Excessive abduction – that is, the affected arytenoid is close to or at maximal abduction (medial aspect of arytenoid at 80° to 90° to sagittal plane, or sometimes even hyperabducted when the apex of the affected corniculate process appears to be displaced beyond the midline, to the normal side of the larynx) |
| 2 | A high degree of arytenoid abduction (arytenoid at 50° to 80° to the sagittal plane) – that is, less than complete abduction |
| 3 | A moderate degree of arytenoid abduction – that is, arytenoid at around 45° to the sagittal plane |
| 4 | A slight degree of arytenoid abduction – that is, arytenoid is slightly more abducted than the normal resting position |
| 5 | No detectable arytenoid abduction present |
| (Dixon, 2003) | |
Loss of abduction by at least one grade is expected in up to 76% of horses within the first six weeks postoperatively (Barnett et al, 2013a), therefore it may be desirable to aim for a greater degree (grade 1) of abduction during surgery, although this must be balanced against a potential increased risk of postoperative coughing and dysphagia (Kidd and Slone, 2002; Dixon et al, 2003).
The optimal degree of abduction is, therefore, subject to considerable debate. It has also been suggested the prevalence of other airway abnormalities may increase following laryngoplasty (Leutton and Lumsden, 2015).
Standing laryngoplasty is gaining popularity, avoiding the risks of general anaesthesia, improving surgical access and visualisation, as well as the surgeons’ assessment of intraoperative abduction (Rossignol et al, 2015).
Given the variable efficacy and potentially high complication rate, alternative surgical treatments for RLN have been investigated. “Laryngeal reinnervation” techniques have been developed in more recent years, with the nerve-muscle pedicle graft (Ducharme, 1989) and direct nerve implantation techniques (Rossignol et al, 2018) being used with some success.
Perhaps the biggest limitation of these procedures is the variable, and sometimes lengthy, time from surgery to return to athleticism. Although reinnervation can be observed as early as 12 weeks postoperatively in some horses, others may not demonstrate successful reinnervation for as long as 12 months after surgery (Rossignol et al, 2018). This is undesirable in some disciplines where time pressures exist to compete at a young age.
Most of the aforementioned procedures are combined with some variation of unilateral or bilateral ventriculocordectomy, which may result in some improvement in airway mechanics, respiratory noise production (Brown, 2003) and performance in a subset of horses. It is unlikely to afford significant improvement as the sole procedure for racehorses with grade 3 and 4 laryngeal function.
Palatal dysfunction: palatal instability and dorsal displacement of soft palate
Palatal instability (PI) has been reported during exercising endoscopy in several studies (Allen and Franklin, 2010; Kelly et al, 2013) and may occur alone or as a precursor to DDSP.
Intermittent DDSP (iDDSP) is arguably a more significant form of palatal dysfunction, potentially responsible for career-limiting poor performance (Barnett, 2018). Diagnosis relies on OGE; however, prolonged DDSP at rest, a hypoplastic epiglottis, palatal billowing on nasal occlusion or swallowing, and ulceration of the caudal border of the soft palate (Lane et al, 2006) are suggestive of iDDSP.
A paucity of evidence-based treatment recommendations exists. Associated abnormalities – such as subepiglottic cysts, granulomas or epiglottitis – should be addressed first if they are present. Non-surgical management is often preferred in the first instance. For example, upper airway inflammation should be treated with anti-inflammatories (topically and/or systemically), and unfit or immature horses should be conditioned and re-evaluated before surgical intervention is considered.
Some evidence supports the use of “tongue-ties”, with success rates of 53% to 61% reported for treatment of naturally occurring disease, as part of medical management strategies (Barakzai and Dixon, 2005; Barakzai et al, 2009a), but a positive mechanical effect has not been documented in normal horses (Cornilesse, 2001).
Surgical treatments include thermal cautery of the soft palate, sternothyroid myotenectomy (Llewellyn procedure) or laryngeal “tie-forward”, and are often combined. Thermal cautery has questionable efficacy as mono therapy (Barakzai et al, 2009a).
Laryngeal tie-forward has the best reported success rate, with approximately 80% of treated horses demonstrating significantly improved racing performance (Woodie et al, 2005). The procedure is usually combined with sternothyroid myotenectomy, and sometimes thermal cautery of the soft palate.
Equine asthma
Equine asthma is a syndrome that encompasses a spectrum of disease of varying severity. Mild equine asthma (formerly inflammatory airway disease) primarily affects younger horses (two to four years of age), although it can occur in horses of any age (Cian et al, 2015).
Horses with mild equine asthma may exhibit mild exercise intolerance and cough during exercise, with cough being variably present at rest (Mazan, 2018; Richard and Robinson, 2016). Marked equine asthma (formerly recurrent airway obstruction) typically affects older horses (older than five years of age), and is allergic and cannot be cured (Couëtil et al, 2016), only managed.
Marked equine asthma will result in clinical signs at rest (Mazan, 2015) that may prevent exercise. Cytologically, a spectrum of neutrophilic inflammation in the tracheal wash fluid and/or BALF of horses with equine asthma, with increases in eosinophils and mast cells variably also present (Cian et al, 2015; Mazan, 2018). Tracheal mucus is a consistent finding, regardless of the severity of equine asthma (Mazan, 2015).
Minimising the time spent in a stable environment is the most important component of managing equine asthma (Calzetta, 2018). In summer pasture-associated disease, pollens are thought to be the trigger.
In horses where 24/7 outdoor management/turnout is not possible, steps to minimise exposure to respirable dust in the stable are required (Figure 4); for example, provision of pelleted feed and use of dust-extracted wood chip bedding (Mazan, 2018). Hay or chaff should be dampened down or steamed and fed from the ground to remove or reduce respirable particles.

Affected horses (if not all horses) should be removed from the building during mucking out, feeding or any other activities that may increase exposure to dust and particulate matter (Mazan, 2018).
Therapeutic management is unlikely to be successful without effective environmental control (Mazan, 2015, 2018; Couëtil et al, 2016), but typically includes provision of glucocorticoids to reduce airway inflammation, with or without addition of bronchodilators.
Inhaled glucocorticoid therapy is preferred to systemic treatment, as the drug is preferentially delivered to the respiratory tract (Haspel et al, 2018). According to a meta-analysis on the available literature, glucocorticoid treatment significantly improves equine asthma, with no difference in efficacy between systemic and inhaled administration of the medication.
However, a difference in the rate of response has been noted, with systemic administration inducing a more rapid response than inhaled medications. The same meta-analysis failed to identify a difference in efficacy between drug delivery via metered dose inhalers or nebuliser (Calzetta, 2018).
Metered dose inhalers provide an easy-to-use treatment method that is generally well-tolerated. Spacer devices are required and have been designed for horses. Human paediatric spacers are a cost-effective alternative.
Inhaled fluticasone is as effective as systemic dexamethasone in controlling clinical signs in horses with mild equine asthma (Léguillette et al, 2017) and is the most effective of the inhaled formulations of glucocorticoid with the longest duration of action. While other studies have found conflicting results on improvement of BALF neutrophilia with both fluticasone and dexamethasone, improved airway hyperreactivity is a consistent finding with both medications (Mazan, 2018).
Bronchodilators can also be administered via inhalation to provide direct administration to the airways; however, in the mild or chronic case that is suffering poor performance, they may offer little benefit over treatment with glucocorticoids alone.
In the authors’ experience, compliance with metered dose inhalers is often poor and results are less consistent than with the use of a nebuliser. Nebulisation has become a popular means of managing equine asthma (Figure 5).

While a considerable cost is associated with the purchase of a nebuliser, the ongoing treatment cost is markedly reduced compared to either systemic or metered dose-inhaled treatment.
Provided they are disinfected effectively, nebulisers can be used for multiple horses. Human research has demonstrated similar efficacy of nebulised dexamethasone to oral prednisolone in management of asthma, and in horses there is little absorption and minimal effect on the hypothalamic-pituitary-adrenal axis associated with treatment, thereby reducing the risk of adverse effects compared to systemic treatment (Haspel et al, 2018).
Inhalation of injectable dexamethasone preparations is well tolerated and does not incite an inflammatory response (de Lagarde et al, 2014). Injectable dexamethasone is used by the authors at 20% of the systemic dose when nebulised, and is diluted in an equal volume of saline.
Fluticasone may be perceived to be more effective than dexamethasone, but is harder to obtain and more expensive. All inhaled medications are used off licence and should be used with appropriate consent in accordance with the cascade.
Conclusion
Accurate history taking and clinical examination are of paramount importance when investigating respiratory tract disease and aid in targeting diagnostics.
Endoscopic examination of the upper and lower respiratory tract is typically required with overground endoscopy, and lower airway washes being required to confirm and further characterise upper and lower respiratory tract disease respectively.
Treatment and prognosis will be dictated by the nature and severity of disease.
